
July 10 was Chronic Disease Day, our annual observance of all that we as chronic disease patients have in common.
Considering last week's passage of the "One Big Beautiful Bill" (OBBB), we modified our "State of the Patient" event to focus on the implications of the bill on state legislatures and how we can keep patients at the center of healthcare policy— despite changing resources. But first:
2025 Legislative Sessions
The Chronic Disease Coalition (CDC) works with MultiState to track and analyze federal and state legislation. We tracked more than 1,500 bills in all states, and MultiState was there to review the legislative trends in our key areas of access to care, affordability and representation. Important gains were made in all areas, but this was not a year for major legislative movement as many legislators were also navigating the uncertainty of the new administration. While Congress stretched out the implementation timeline of the OBBB, navigating the changes over the next five to 10 years will still be a major undertaking.
The Multi-Year Approach for OBBB Implementation
The hottest part of our conversation was around the timeline and implications for states.
“There are significant state legislative implications, state administrative implications and state budget implications that are tied to this,” said MultiState’s Brock Ingmire. “This bill is the most disruptive policy intervention to healthcare since the ACA…It will have ripple effects for states over the next 10 years related to healthcare and non-healthcare policy interventions.”
Medicaid funding may come from the federal government, but it's a state program and legislators are going to have major work to do over the next couple of years. Their work will also drive major changes to the patients, insurers, and the provider community.
The good news is that not everything happens at once. That's why it's important to consider the timeline and prepare to guide state policy from the beginning.
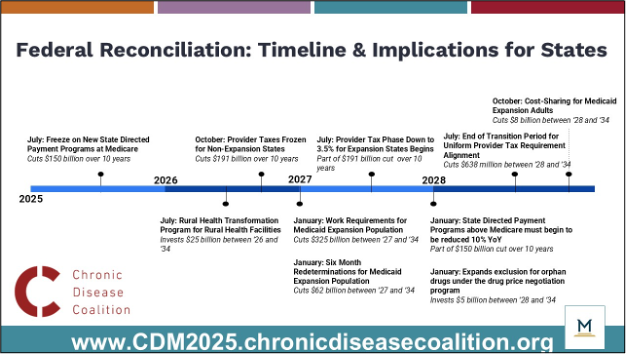
Knowing that people and health care providers in rural areas are highly dependent on Medicaid and Medicare coverage, Congress planned for rural health facility investments to start in 2026.
At the same time, states that are highly dependent on provider taxes to keep hospitals and other facilities afloat will start to see changes.
Work requirements, coming into play in 2027, will be the first direct patient-focused change that many people will see and experience. Brock Ingmire of MultiState made the point that many states do not have the infrastructure or staff to manage the six month redetermination requirements, and that will likely be a budget problem that they will have to solve immediately. That said, there are a lot more technical questions that the Centers for Medicare & Medicaid Services (CMS) will have to answer as part of its rulemaking process over the next several years.
"North Star" Care: Patients First, Progress Together
So where do we go from here?
In times of shrinking resources, it's too easy for various parts of the healthcare system to fight over scraps. But reduced budgets don't change the need for better health outcomes delivered in more affordable and accessible ways. There's widespread recognition that chronic disease in the United States carries an enormous human and financial toll. Even if you personally do not have a chronic disease, that toll is carried by everybody.
That's why it's essential that we work to prioritize high value care. There are ways to improve health and reduce health care expenditures over time. Strategies like the ones below keep people healthy, working, caring for their families in communities.
Strategies for Keeping People Healthy, Working & Caring for Their Families
- Primary care, good disease management and care coordination allows for early intervention and better management of chronic conditions
- Preventive care like the Diabetes Prevention Program, vaccines and regular screenings can also keep infectious diseases from becoming chronic diseases and allow for the early intervention that saves money and lives
- Home-based and other site-of-care delivery eases the burden on patients and reduces the need for large facilities
- Behavioral health integration
- Payer alignment
- Telehealth
Want to Learn More?
Watch the video here with passcode @fYy8ymJ.
Additional Resources
- View the CDC's 2025 Roll Call of Champions
- Read our latest newsletter and subscribe here to receive our twice-monthly updates
- Read our Policy Priorities
- Send a letter to legislator for Chronic Disease Month
- See other letters you can send to legislators on Medicaid and mental health.