3.21.16
As the cost of health insurance premiums has risen over the years, some chronic disease patients need help to pay their bills, and often they can turn to nonprofits for assistance – much like the financial assistance programs that help people in need keep the lights and heat on in their homes. The American Kidney Fund’s premium assistance program is among these programs, helping 79,000 economically disadvantaged kidney patients to pay their health care premiums.
But the AKF program for kidney patients is now under threat from insurance companies using a range of tricks to avoid accepting premium assistance payments, such as:
- Requiring patients to promise they will not accept assistance from certain nonprofit organizations as a condition of enrollment
- Inaccurately telling patients that federal regulations prevent them from accepting premium assistance
- Preventing patients from signing up for a new plan by providing abrupt notice at the end of open enrollment periods that a selected insurance plan will not accept third-party payments
- Telling patients that accepting third-party premium assistance in any form is grounds for coverage termination
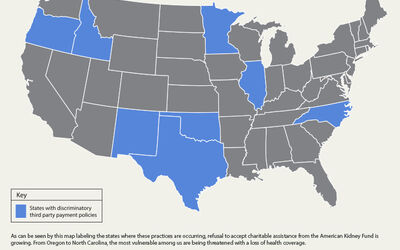
Our third-party payment ban map shows just some of the states where we know this harmful practice is occurring. Discrimination is taking place across the country, including in:
- North Carolina: Insurers are rejecting third-party premium assistance for qualified health plans on the state’s health insurance exchange as well as the Medigap plans.
- Oregon: Third-party premium assistance is being refused by insurers, and insurance companies have asked some patients to sign letters of attestation stating that they will not accept assistance from groups such as the American Kidney Fund.
- Minnesota: Insurers have given patients abrupt notice at the end of open enrollment that they do not accept third-party premium assistance, giving patients little to no time to find other forms of coverage.
- Illinois, New Mexico, Oklahoma and Texas: Insurers have used ambiguity in federal regulations as a reason for rejecting third-party premium assistance.
What’s next?
Third-party premium payment bans certainly aren’t the only way insurance companies are discriminating against those with chronic health conditions, but they are an increasingly prevalent tactic.
We know from other groups, including the National Hemophilia Foundation, that this is an issue for other patients too. Click here to see a letter from hemophilia advocates about this.
Other states and chronic diseases could be next.
If you’d like to learn more about the issues in your state or to tell us your concerns, please sign up for the Chronic Disease Coalition today.
Additional information: American Kidney Fund Fact Sheet